Understanding Ventricular Assist Device (VAD) Implantation: A Comprehensive Guide
Introduction to Ventricular Assist Device Implantation
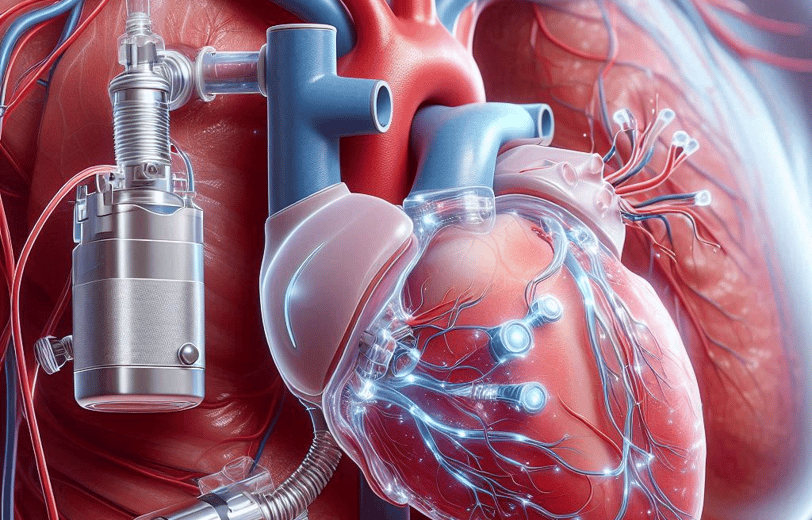
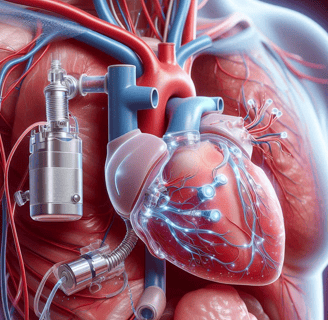
Ventricular Assist Devices (VADs) are sophisticated medical devices designed to support heart function and blood flow in individuals suffering from severe heart failure. These devices are surgically implanted into patients whose hearts are no longer capable of pumping blood effectively on their own. VADs serve as a crucial intervention for those awaiting heart transplants, as well as for patients who are ineligible for transplant but require long-term support.
A VAD operates by taking over the pumping function of either the left or right ventricle. The most commonly used type is the Left Ventricular Assist Device (LVAD), which aids the left ventricle in delivering oxygen-rich blood to the body. Alternatively, the Right Ventricular Assist Device (RVAD) supports the right ventricle in pumping blood to the lungs for oxygenation. In some cases, a Bi-Ventricular Assist Device (BiVAD) may be employed to assist both ventricles simultaneously.
The fundamental components of a VAD include a pump, a power source, and a control system. The pump is implanted in the chest or abdomen and is connected to the heart by a series of tubes. The power source, typically external, is connected through a driveline that exits the body, while the control system regulates the pump's operation. Modern VADs are designed to be portable, allowing patients to maintain a degree of mobility and quality of life during treatment.
Understanding the role and functionality of VADs is essential for patients and healthcare providers alike. These devices not only improve survival rates but also enhance the quality of life for individuals with severe heart failure. By offering a mechanical solution to a critical physiological problem, VADs represent a significant advancement in cardiac care and a beacon of hope for those affected by debilitating heart conditions.
Why Ventricular Assist Device Implantation Might Be Needed
The necessity for a Ventricular Assist Device (VAD) implantation often arises in the context of severe cardiovascular conditions that impair the heart's ability to pump blood effectively. One of the primary indications for VAD implantation is end-stage heart failure. This condition, also known as advanced heart failure, occurs when the heart's ventricles are no longer capable of maintaining adequate circulation to meet the body's needs. Patients suffering from end-stage heart failure often experience debilitating symptoms such as extreme fatigue, shortness of breath, and fluid retention, significantly impacting their quality of life.
Another critical condition necessitating the use of a VAD is cardiomyopathy, a disease of the heart muscle that results in its weakening or structural changes. Cardiomyopathy can be of various types, including dilated, hypertrophic, and restrictive, each presenting unique challenges. Regardless of the type, the common outcome is a compromised ability of the heart to pump blood effectively, leading to severe heart failure. In such scenarios, a VAD can provide essential circulatory support, alleviating symptoms and improving patient outcomes.
Moreover, VADs play a crucial role as a bridge to heart transplantation. For patients awaiting a heart transplant, a VAD can sustain them through prolonged waiting periods, ensuring they remain viable candidates for surgery. This interim support is vital, as it stabilizes patients and often improves their overall condition, making them better prepared for the eventual transplant procedure.
In some cases, a VAD may be employed as a destination therapy, serving as a long-term solution for patients who are not candidates for heart transplantation. For these individuals, a VAD can significantly enhance life expectancy and quality of life, providing a sustainable option for managing chronic heart failure.
The life-saving potential of VAD implantation cannot be overstated. By restoring adequate blood flow and relieving the burden on the heart, VADs offer a beacon of hope for patients grappling with severe heart conditions, underscoring the transformative impact of this medical intervention.
Diagnosing the Need for a Ventricular Assist Device
The decision to implant a Ventricular Assist Device (VAD) is a critical one, requiring a comprehensive diagnostic process to evaluate the patient's condition accurately. Various diagnostic tools and tests are employed to determine the necessity for a VAD, ensuring that the patient receives the most appropriate treatment.
One of the primary diagnostic tools used is the echocardiogram. This non-invasive imaging technique utilizes ultrasound waves to create detailed images of the heart's structure and function. By assessing parameters such as ejection fraction and ventricular size, cardiologists can gauge the severity of heart failure and the heart's pumping capacity. A significantly reduced ejection fraction often signals the need for further intervention, including the potential implantation of a VAD.
Magnetic Resonance Imaging (MRI) is another crucial diagnostic tool. MRI provides high-resolution images of the heart and surrounding vessels, offering detailed insights into myocardial tissue health, scarring, and blood flow patterns. This information is vital in determining whether the patient's heart muscle can recover with medical therapy alone or if mechanical support through a VAD is necessary.
Blood tests also play a pivotal role in the diagnostic process. Biomarkers such as B-type natriuretic peptide (BNP) and N-terminal-proBNP are indicative of heart failure severity. Elevated levels of these biomarkers suggest increased cardiac stress and dysfunction, prompting further evaluation for potential VAD implantation.
In addition to diagnostic tests, clinical signs and symptoms are essential indicators of the need for a VAD. Patients often present with pronounced shortness of breath, which may occur even at rest or with minimal exertion. Fatigue and general weakness are common, significantly impairing daily activities. Fluid retention, manifested as swelling in the legs, abdomen, and lungs, is another critical symptom indicating advanced heart failure. These clinical manifestations, in conjunction with diagnostic findings, guide the decision-making process for VAD implantation.
Ultimately, the comprehensive diagnostic evaluation integrating echocardiograms, MRIs, blood tests, and clinical symptoms ensures that the indication for a Ventricular Assist Device is thoroughly substantiated, optimizing patient outcomes.
Pre-Surgery Considerations and Preparation
Before undergoing the implantation of a Ventricular Assist Device (VAD), it is crucial to undertake several pre-surgery considerations and preparations. A comprehensive preoperative evaluation is essential. This typically involves a series of tests and assessments to determine the patient's overall health and suitability for the procedure. Common evaluations include blood tests, electrocardiograms (EKG), echocardiograms, and possibly a cardiac catheterization. These tests help the medical team understand the functioning of the heart and identify any potential risks associated with the surgery.
Consultations with cardiologists and surgeons play a pivotal role in the preparatory stage. During these consultations, patients are informed about the benefits and risks of VAD implantation, the surgical process, and the expected recovery trajectory. This is also an opportunity for patients to ask questions and clarify any concerns they might have. In some cases, a multidisciplinary team including nutritionists, psychologists, and physical therapists may be involved to ensure a holistic approach to the patient's care.
Necessary lifestyle changes are often recommended in the lead-up to the surgery. These changes can include dietary adjustments to improve overall health, cessation of smoking to enhance lung function, and moderating alcohol consumption. Patients may also be advised to engage in light physical activities, as tolerated, to maintain a level of fitness that can aid in a smoother recovery post-surgery.
On the day of the surgery, specific preparations are required. Patients are usually instructed to fast for a certain period before the operation to reduce the risk of complications during anesthesia. Medication adjustments are also common, and patients need to follow the guidance of their healthcare provider regarding the continuation or temporary cessation of certain drugs. Mental preparation is equally important, as undergoing a significant procedure like VAD implantation can be psychologically taxing. Support from family, friends, and counseling services can be invaluable during this time.
Overall, meticulous pre-surgery considerations and preparation are fundamental to the success of VAD implantation. By adhering to medical advice and making necessary adjustments, patients can enhance their readiness for the procedure and improve their chances of a favorable outcome.
Post-Surgery Care and Recovery
Following the implantation of a Ventricular Assist Device (VAD), the immediate post-operative care is crucial to ensure a smooth recovery. Patients can expect to spend several days in the intensive care unit (ICU), where they will be closely monitored by medical professionals. During this period, vital signs such as heart rate, blood pressure, and VAD function are observed continuously to detect any abnormalities promptly. Pain management is also a priority, with medications administered to alleviate discomfort.
The recovery timeline varies for each individual but generally spans several months. Initial recovery involves gradual reduction of ICU monitoring and transition to a regular hospital room. Patients are encouraged to begin light physical activity under supervision to promote circulation and prevent complications such as blood clots. Once discharged, the patient will need to adhere to a structured rehabilitation program that includes physical therapy to regain strength and improve cardiovascular health.
Potential complications post-surgery include infection, bleeding, blood clots, and device malfunction. It is essential for patients and caregivers to be aware of the signs of these complications, such as fever, unexplained pain, or unusual sounds from the VAD. Prompt medical attention is necessary if any of these symptoms occur.
Lifestyle adjustments are also vital for successful recovery. Patients must adopt a heart-healthy diet, quit smoking, and manage co-existing conditions like diabetes or hypertension. Regular follow-up visits with the healthcare team are critical to monitor the VAD’s function and the patient’s overall health. These visits typically involve blood tests, imaging studies, and device evaluations.
Incorporating these practices into daily life will enhance the recovery process and ensure the optimal functioning of the VAD. By adhering to medical advice and maintaining a proactive approach to health, patients can achieve a better quality of life post-implantation.
Medtu Care: Facilitating Top-Quality VAD Treatment in Indore
Medtu Care stands out as a distinguished facilitator of Ventricular Assist Device (VAD) treatments in Indore. Widely recognized for its commitment to exceptional healthcare, Medtu Care collaborates with renowned doctors and premier hospitals in the city, ensuring that patients receive top-notch medical care. Indore, celebrated as the cleanest city in India, provides an optimal environment for recovery, complementing the advanced medical services offered.
Choosing Medtu Care for VAD implantation comes with multiple advantages. Patients gain access to a network of experienced doctors who specialize in VAD procedures. These medical professionals bring a wealth of expertise and a proven track record of successful outcomes, ensuring that every patient receives the highest standard of care. The hospitals affiliated with Medtu Care are equipped with state-of-the-art facilities, enabling the use of cutting-edge technology in VAD treatments.
Affordability is another significant benefit of opting for VAD treatment through Medtu Care. By negotiating competitive rates with top-tier hospitals, Medtu Care makes high-quality medical care accessible to a broader demographic. This balance of excellence and affordability positions Medtu Care as a preferred choice for those seeking VAD implantation in Indore.
In summary, Medtu Care's dedication to facilitating top-quality VAD treatment in Indore is evident through its collaboration with experienced doctors, state-of-the-art hospital facilities, and a commitment to affordability. Patients can trust Medtu Care to provide comprehensive support and care, ensuring positive treatment outcomes and a smooth recovery journey.